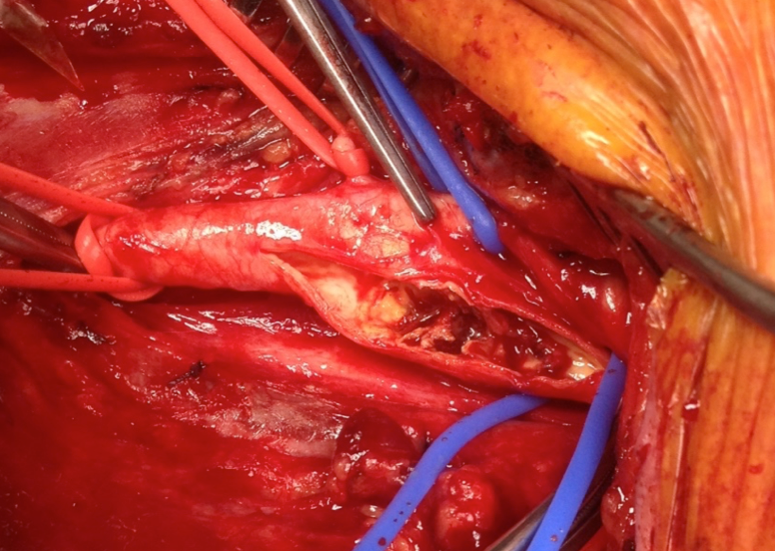
Carotid Endarterectomy (CEA)
The carotid endarterectomy is the surgical removal of a plaque build up within the carotid artery. The buildup typically occurs where the common carotid artery bifurcates to form the internal and external carotid arteries. Atherosclerosis causes plaque to be deposited along the inside of the artery wall. As plaque builds up in the lumen, blood flow through the artery is restricted, a condition known as carotid stenosis. When the stenosis reaches 50%, the stenosis is considered moderate. With moderate to severe stenosis, a carotid endarterectomy may be indicated to remove the plaque.
Why Neuromonitoring…
There are several events during the surgical procedure that warrant monitoring. The first occurs during dissection of the artery. Its necessary to expose and release the artery above and below the bifurcation. In this region there are several cranial nerves that are at risk. The facial, the vagus and the hypoglossal nerves are all in close proximity to where the surgeon must dissect out the carotid artery. Each of these nerves innervate muscles making it possible to monitor their integrity using electromyography (EMG). Hypoglossal nerve injury is the most common and occurs in about 5% of the cases [1]. The next event is typically the primary reason neuromonitoring is performed during CEA surgery. Before the surgeon opens up the segment of the internal carotid artery to remove the plaque, a clip is placed farther downstream on the internal artery. This shuts down blood flow to the ipsilateral anterior portion of the brain. In healthy individuals, collateral circulation compensates by providing flow from the contralateral circulation through the circle of Willis. However, there are anatomical variations to the circle of Willis, which in a small percentage of people prevent collateral circulation. Continuous monitoring of cortical somatosensory evoked potentials (SSEPs) and electroencephalograms (EEGs) enables the neurophysiologist to alert the surgeon immediately if collateral circulation is not present.
1. European J Endov Surg 2104; 47(1): 2-7